In Western Europe and North America, prostate cancer (PCa) is the most commonly diagnosed cancer in men and the second leading cause of cancer-related death. Prostate cancer is a highly heterogeneous disease, and to date, most treatment algorithms have been based on clinical risk stratification based on tumor stage (T-stage), prostate specific antigen (PSA) level at diagnosis, and Gleason grading group (GG). Although this clinical risk stratification has been shown to be prognostic and predictive, better biomarkers are still needed to improve patient stratification.
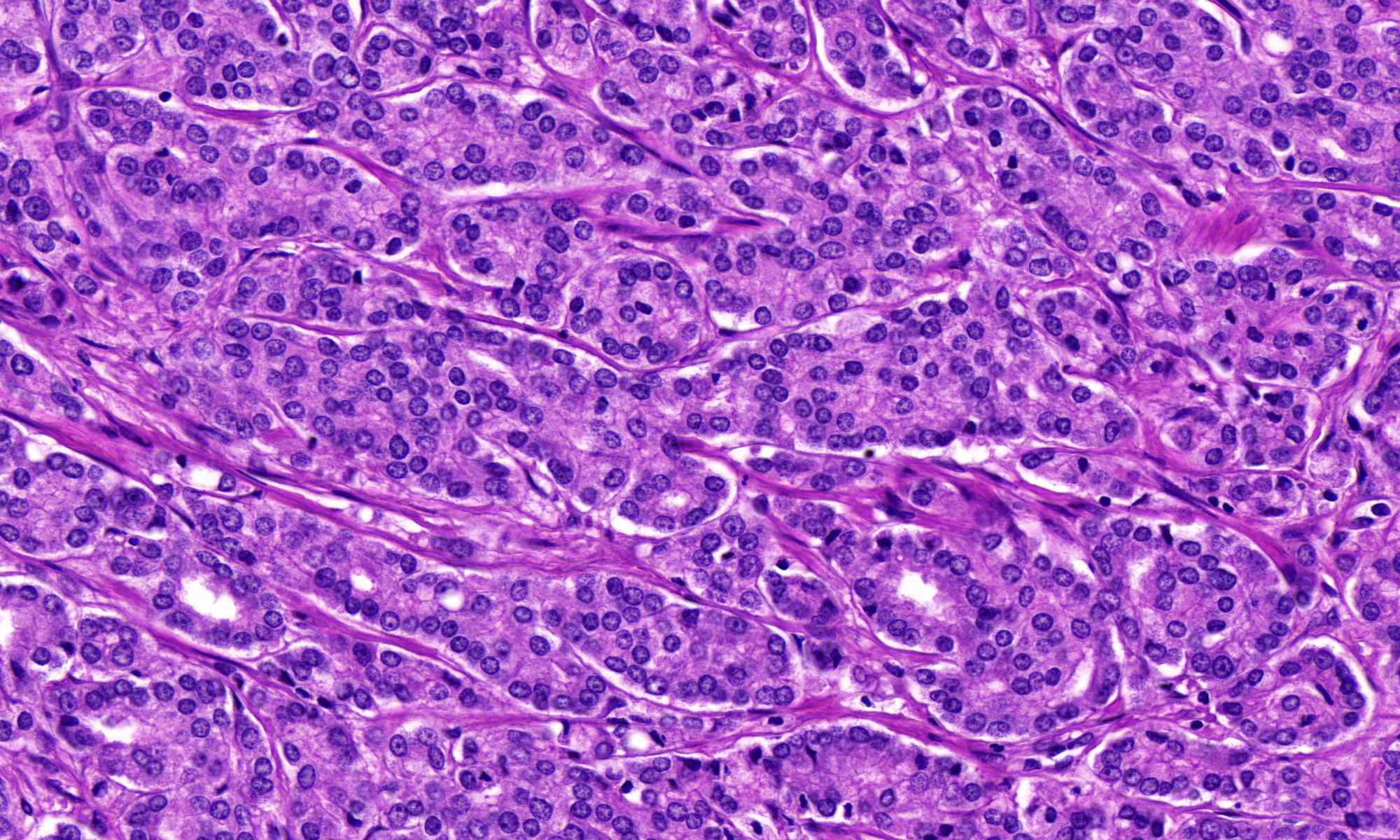
Gleason score (GS) is a classification of the histologic growth pattern of prostate adenocarcinomas. The overall GS (from 6 to 10) is the sum of the two most common predominant patterns (from 1 to 5) in the sample. For finer stratification, the International Society of Urologic Pathology (ISUP) developed a new classification into five GGs to distinguish GS 7(3+4) (referred to as GG2 in the 2014 ISUP) from GS 7(4+3) (GG3). In 2019, further ISUP changes were taken up for PCa grading, which recommends reporting the percentage of GS4 patterns in each case of GG2 or GG3.
Despite all these changes, both the GS and GG grading systems still have some uncertainties. Especially the group of GG2 (Gleason 3 + 4) PCa patients is currently still actively treated according to the guideline recommendation, although some of the patients are overtreated with this therapeutic strategy.
Thus, there is an urgent need to develop better molecular and genetic prognostic biomarkers that can be interpreted in combination with clinicopathologic features. These include metabolome-based biomarkers, mRNA-based blood-based biomarkers, urine biomarkers, and genetic tissue-based biomarkers. Of note, of the plethora of biomarkers being researched, only 2 have so far been approved by the FDA for specific indications (PCA3 and Polaris). In Europe, none of these tests for prostate cancer has yet been established in clinical care.
The aim of the PROSurvival project is to test whether artificial intelligence (AI) can be used to identify patterns from histo-pathological images that can be used to improve the prediction of biochemical cancer recurrence or patient survival. Thus, the goal is to identify those patients who can safely forgo active therapy in the future or who absolutely need active therapy.